A crisis is hitting your local drugstore. Why the slow demise of a 130-year-old family-owned pharmacy chain spells disaster for consumers
Sometimes Seattle earns its gloomy reputation. It was cold, dark, and wet on the February morning I arrived, and I needed a new umbrella.
This should have been a temporary inconvenience, at worst. Seattle—home base to Amazon, Microsoft, Costco, Starbucks—is one of our nation’s most important commercial hubs, and one of its wealthiest cities. Surely there would be several drugstores downtown, eager to sell me new rain gear.
But many of the stores I walked past were long closed, or filled with shelves that alternated between empty and locked-up. Finally I came to the darkened entrance of what was, until December, store No. 1 of Bartell Drugs, a beloved local chain now owned by Rite Aid. One of the windows still had the Bartell’s logo and a sign declaring it was “Est. 1890”; taped above them was a “For Lease” poster. Signs on the door told customers their prescriptions had been transferred to the Walgreens up the street. Huddled under a dirty white blanket, a person slept in the entryway.
“It’s heartbreaking,” says Ryan Oftebro, an owner of Kelley-Ross, one of the last remaining general-purpose pharmacies in downtown Seattle. “Bartell’s was community-focused and local, and that’s where you went for high-quality service.”
Bartell’s, as everybody calls it in Seattle, was passed down from father to son to grandchildren over 130 years before the Bartell family sold it to Rite Aid in 2020. By then, the business had 67 locations, annual revenues of $550 million, and the title of the country’s oldest family-owned pharmacy. Even today, walking into one of the roughly 40 remaining Bartell’s feels like entering a time portal to the days of soda fountains and the neighborhood pharmacist who knew your kids’ names and the dates of their last colds: friendly clerks, folksy signs, aisles full of toys and chocolates. “Bartell’s has always been more than a drugstore,” one of many columnists lamenting its fate recently wrote. “It is part of the fabric of Seattle.”
And now it’s dying. Rite Aid declared bankruptcy in October, and since then it has said it will close more than 520 stores. The casualties include a third of the Bartell Drugs locations in the region, one of which was the last 24-hour pharmacy operated by any company in downtown Seattle: Today, anyone who wakes up in the middle of the night seeking cold medicine, or help for a child with an ear infection, has to go to an emergency room or drive to another neighborhood.
Across the state, the rate of annual pharmacy closures has doubled since 2022. Since 2008, an average of 30 pharmacies per year shut down, according to the Seattle Times. But over a period of 13 months ending in early March, 81—more than 8% of all Washington pharmacies—have gone out of business, according to the Washington State Pharmacy Association.
It’s a microcosm of a crisis that extends far beyond the Pacific Northwest. American drugstores are caught in a perfect storm of factors: The wide-ranging retail apocalypse has made it more difficult than ever for brick-and-mortar businesses, with their expensive rents and staffing costs and post-pandemic fears about retail crime, to compete with Amazon and other low-overhead online sellers. For pharmacies in particular, the grim shadow of the opioid crisis has saddled the large chains with lawsuits and multibillion-dollar settlements, while overworked and burned-out pharmacists are fleeing the industry in droves. Meanwhile, they say the health insurance companies that decide how much pharmacies actually get paid have been tightening the screws, inexorably reducing their reimbursements for prescriptions.
“Pharmacies are in shambles. It’s unbelievable what’s happening right now,” says Abdikadir Athur, a pharmacist who spent six years at Bartell’s and then Rite Aid before cofounding a small pharmacy, Tukwila Station, in the Seattle suburb of SeaTac.
He adds: “If even big chains cannot survive—and even CVS and Walgreens are hurting—what do you expect for the small pharmacies?”
Indeed, the big drugstore chains are suffering—at least when it comes to the pharmacy services at the core of their companies. CVS and Walgreens are making less money on an annual basis from filling prescriptions, and are betting on other businesses for growth. Rite Aid, trying to claw its way out of debt, is getting out of every drugstore lease it can.
CVS, Walgreens, and Rite Aid have announced the closures of more than 1,500 stores. (CVS says its closures of 900 stores over three years were partially to reduce overlap, while Walgreens is closing 200 U.S. stores as a cost-cutting measure; spokespeople for both companies say the vast majority of Americans will still live within five to 10 miles of one of their stores. A Rite Aid spokesperson said that the company is closing underperforming stores “to further reduce rent expense and strengthen overall financial performance.”)
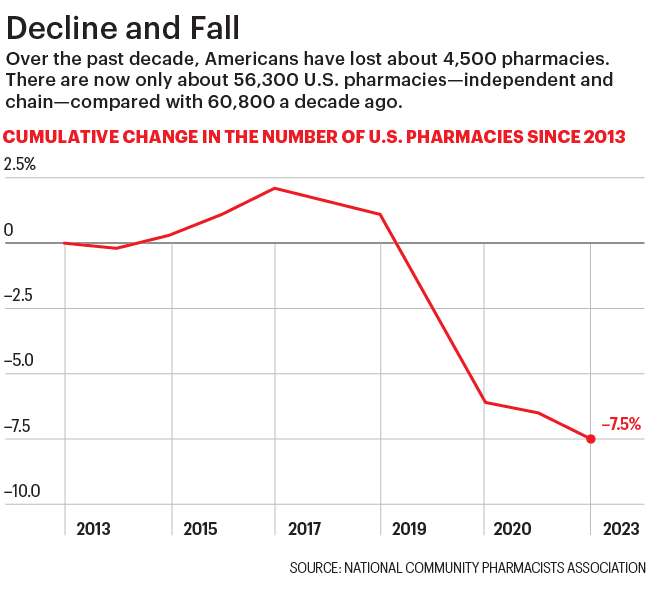
Those closures are contributing to a larger, industrywide decline. In 2023 there were about 4,550 fewer pharmacies than a decade earlier, according to the National Community Pharmacists Association—and industry analysts say those numbers don’t reflect the true impact on smaller and independent pharmacies. The trade group also warned in February that several thousand more local pharmacies, up to a third of its members, could close this year. And that was before the massive Change Healthcare hack snarled insurance reimbursements, upending many pharmacies’ cash flow. (See our story, “America’s health system is still in crisis after its biggest cyberattack ever—but the ‘catastrophe’ is just a blip for the giant company that got hacked,” also from this issue.)

Independent providers blame the powerful pharmacy benefit managers (PBMs) owned by large health care companies—including CVS and UnitedHealth Group—for squeezing the amount they get paid and making it difficult to turn a profit. “There’s always been downward pressure on reimbursements,” says Oftebro. “But the tipping point has really been in the last year or two.”
The gathering tsunami of pharmacy shutdowns highlights a worsening national crisis for the United States, where health care is the most expensive in the world. As U.S. health care companies continue getting bigger and more consolidated, while the number of primary care doctors shrinks, pharmacies could have filled in some of the gaps. Instead, they’re becoming dystopian nightmares—or vanishing entirely.
Pharmacists across the nation, especially at the big chains, are walking out and raising alarms about understaffing and increased workloads, which they say could harm patients. Many have dropped out of the industry altogether: Some pharmacists who have fled retail tell Fortune that “it’s not a desirable profession anymore.” And fewer and fewer people are entering the field: Only 13,323 new pharmacists graduated in 2022, down from 14,223 a year earlier and the largest drop in new graduates since 1983, according to the American Association of Colleges of Pharmacy. (Spokespeople for CVS and Walgreens tell Fortune that they are listening to their pharmacists’ concerns and investing in addressing them, including by increasing staffing and recruiting.)
In other corners of retail, e-commerce has filled in the gaps left by brick-and-mortar declines. But for pharmacies, the high-tech solutions—including direct-to-consumer pharmacies such as Capsule, GoodRx, and Mark Cuban’s Cost Plus Drugs—haven’t yet been widely embraced. In 2023, mail-order pharmacies delivered less than 9% of U.S. 30-day prescriptions, according to the Drug Channels Institute.
Ultimately, this harms all consumers—with those who are already most underserved and vulnerable paying the biggest price. As Seattle’s drugstore ecosystem shuts down, “it’s creating pharmacy deserts that shouldn’t exist in urban places,” says Ryan Hansen, a pharmacist and professor serving as interim chair of the University of Washington’s pharmacy department.
“We’ve got Amazon,” he adds, “but we don’t have pharmacy.”

For a brief, shining moment, COVID-19 seemed like it would revitalize American pharmacies as the fix to our most pressing health care problems. COVID testing and then the government-subsidized vaccine push gave the CEOs of CVS and Walgreens a national platform to promote their pivots toward buying up primary care providers and other doctors’ offices.
The pandemic initially had a halo effect on all pharmacies, including local chains and independents. COVID testing and treatment was a visible model of how pharmacists could become more effective frontline health care practitioners, delivering accessible, convenient, and affordable care for simple ailments—harking back to the old days of the American corner drugstore.
“We were very happy in the COVID pandemic, when we had 60,000 pharmacies willing to provide vaccines,” says Inma Hernandez, a professor of clinical pharmacy at UC San Diego. “And we know that there’s a lot more to pharmacy access than just getting a drug—it’s about interactions with the pharmacist.”
In theory, Bartell’s and its Washington competitors should have been well-positioned to reshape primary care for their communities. State law in Washington empowers pharmacists to prescribe, without always referring patients to a doctor—meaning that it’s one of a handful of states where pharmacies could most easily supplement an overtaxed and shrinking primary care system.
"If even big chains cannot survive … what do you expect for the small pharmacies?"
Abdikadir Athur, co-owner, Tukwila Station Pharmacy
Instead, they found themselves fighting for survival. There are many causes behind the national crisis of retail pharmacies, all of which are particularly acute in downtown Seattle. Behind a futile umbrella hunt, a whole retail kingdom is being lost: The pandemic hollowed out urban centers, as wealthier residents fled for greener remote-work pastures. High-end retailers have followed the money, closing down what they see as undesirable locations, while mass-market drugstore chains have responded to fears about theft and other crime by locking up the toothpaste and deodorant. Those changes drive away more customers and hurt the pharmacies that rely on front-of-store retail operations for up to 40% of their revenues. “When retailers lock up their products to create plexiglass prisons, they lock out their customers,” retail analyst Brittain Ladd says.
But the main problem that pharmacists cite is simple: They’re no longer getting paid enough to stay in business. In the multifront battle to cut costs in America’s expensive health care system, pharmacies say they are shouldering a disproportionate share of the burden.
“That traditional model of that corner drugstore that is just dispensing prescriptions is very difficult, if not impossible, to make work these days,” says Oftebro, adding that at his pharmacies, “reimbursement on the majority of prescriptions is now at or below the acquisition cost of the drugs.”
For this, many blame the middlemen: the pharmacy benefit managers. The three largest PBMs are owned by or affiliated with insurance companies—CVS’s Caremark (which shares a corporate parent with Aetna), UnitedHealth’s Optum Rx, and Cigna’s Express Scripts—and together they control how 80% of all U.S. prescriptions are processed.
The PBMs’ power is part of a bigger story of consolidation. As Fortune reported last year, the relentless M&A and “vertical integration” that have now made CVS and UnitedHealth Group two of the largest companies in the world have concentrated tremendous economic power in the hands of a small number of players.
PBMs say they are able to ease the sometimes-soaring prices set by drug companies. They determine how much patients pay for the medications they’re prescribed and also decide how much they will reimburse pharmacies for buying the drugs—and such reimbursements have been falling for years, pharmacists, executives, and industry analysts note.
Pharmacies in general make money on the margins of the prescriptions they fill, as well as by offering additional clinical services and by selling over-the-counter meds and household necessities, greeting cards, cosmetics, and candy. But the margins on prescriptions have gotten so thin that sometimes there’s no money to be made at all, says an independent Seattle-area pharmacist, who offers this illustration: A common brand-name diabetes drug costs around $590 for the pharmacy to buy. The patient pays $75 at the counter, but their insurance plan only covers an additional $480—meaning that the pharmacy is out $35 for filling this prescription. (Adding to the cash squeeze, the pharmacy may also have to wait weeks for the PBM reimbursement.)
The contracts that determine this pricing are complex, and pharmacists have complained for decades about their lack of transparency, amid their diminishing profits. They also say they don’t have any bargaining power with PBMs’ contracts: If they don’t want to accept the drug prices set by a PBM, they must stop accepting that insurance, meaning they will lose the business—and the ability to serve—the patients covered by that insurance company.
In areas left with only one or two pharmacies, if a pharmacy refuses to accept the insurance that covers a majority of residents, it can be hard for patients to get their medications locally. “I have clients who have gone a week without their [opioid-addiction treatment] Suboxone,” says Meredith Trible, a job-assistance case manager who works with communities in rural eastern Virginia. “And for a lot of rural residents, some of us can’t get delivery all the way to our doors, because of the remoteness of our addresses.”
PBMs and their representatives say, essentially, that pharmacists are crying wolf. PBMs tell Fortune that independent pharmacies do indeed have bargaining power with PBMs, since they generally belong to large pharmacy services administrative organizations that negotiate prices and reimbursements with PBMs on behalf of their members. They argue that independent pharmacists have long made PBMs a convenient scapegoat for all of their business challenges (such as the high costs for small businesses of competing with larger, better-funded chains or low-overhead mail-order alternatives). And they say that PBMs are only negotiating drug prices to save American consumers from the high costs set by Big Pharma manufacturers.
“Accusations that PBMs are forcing pharmacy store closures are unproductive and not based in fact,” Greg Lopes, a spokesperson for PBM lobbyist PCMA, said via an emailed statement. “Pharmacy benefit companies recognize the vital role pharmacies play nationwide to create access to prescription drugs for patients.”
Yet it’s hard to deny the mounting national—and bipartisan—consternation over the impact of PBMs on pharmacies and their patients.
“I’m very concerned about what’s happened in our state, and I definitely think that PBMs have played a role in the closure of some independent pharmacies,” Sen. Maria Cantwell, the Washington Democrat who has cosponsored legislation that would regulate PBMs with Iowa Republican Sen. Chuck Grassley, tells Fortune.
“The situation is now very urgent,” she adds. “When you take a pharmacy out of a neighborhood, and they no longer have that in their community, it’s a real problem.”
CVS, which says there is a “strict firewall” between its pharmacy business and its PBM, Caremark, is navigating both sides of this contentious debate. Its spokespeople tell Fortune that it reimburses independent pharmacies more than it does chains, including its own pharmacies. (The company has also acknowledged in regulatory filings that "continued pharmacy reimbursement pressure" has affected the business results of its pharmacy operations.)
More broadly, and perhaps in light of the mounting attention from Washington, CVS and several other big players dominating health care—on both the retailer and the PBM side—are trying to address some of the issues pharmacists have raised about the PBM model. CVS has recently launched two programs—one for how it gets paid as a pharmacy, and one for how its Caremark reimburses pharmacies—that it says will increase transparency and simplify costs. UnitedHealth’s Optum unveiled a similar program in 2023, and a spokesperson says it is “focused on ensuring pharmacies are paid fairly.” Cigna’s Express Scripts in November also announced a new, simplified payment model, and a spokesperson tells Fortune the PBM is “committed to supporting” the “vital role” independent pharmacies play in health care.
Walgreens’ relatively new CEO, Tim Wentworth, previously ran Express Scripts and has added his voice to the mounting chorus calling for his old industry to change the way it deals with his new one, telling investors in March that Walgreens “welcome[s] any model that reimburses us for the unmatched value we provide patients.”
Still, independent pharmacists without the scale or heft of Walgreens and CVS aren’t holding their breath for a big change. Oftebro, whose father bought Kelley-Ross in 1973, now runs it and two other pharmacies with partners including the University of Washington’s Ryan Hansen. But these days, he says, it’s their specialist operations that pay the bills because they don’t have to deal with PBMs. These include a cash-only compounding pharmacy; a travel clinic; and specialist services for patients seeking treatment for addiction or HIV prevention.
As Bartell’s and other downtown pharmacies shut down, and their customers stream into Kelley-Ross seeking basic and unprofitable prescriptions that take time for his staff to fill, Oftebro says he’s been tempted to close down his general-purpose storefront. “We’re busier than ever, but there’s no margin,” he says. “These are the same prescriptions that close pharmacies.”
When pharmacies lose money and spend staff time on filling high-volume but unprofitable prescriptions, Oftebro adds, “customers can love you to death.”
In 1890 a 21-year-old Kansas pharmacist named George H. Bartell purchased a small pharmacy in central Seattle. Over the next 130 years, as he and his descendants built up a beloved retail hub, the Bartells beat the odds: Family businesses proverbially die within three generations, and small businesses, on average, don’t last a decade.
But by 2020, Bartell’s was struggling. Its front-of-store business was facing increased competition from online retailers, while its pharmacies were trying to survive on smaller and smaller PBM reimbursements. By the time Rite Aid came calling, even though their company was making over half-a-billion dollars in annual revenue, the Bartell family could only get the price up to $95 million—along with a promise that Rite Aid would keep the Bartell name on its stores.
“We felt that this was the only answer,” George D. Bartell, grandson of the founder, told the Seattle Times. “It was getting more difficult for regional operators to compete in the market.”
Almost four years later, the chain’s employees and customers are still reeling. Those close to the Bartell family, who declined repeated interview requests, talk about the Rite Aid sale like the death of a loved one: “I don’t go into Bartell’s anymore. It’s really hard,” says Billy Chow, Bartell’s former vice president of pharmacy and now head of operations for health care tech startup Prescryptive Health.
Meanwhile, the chain’s purchaser was facing its own struggles: In October 2020, Rite Aid was running a distinct third to CVS and Walgreens. It had been shrinking for years, especially after a failed effort to merge with Walgreens, and was carrying a load of debt. As state attorneys general started suing pharmacy chains over their pharmacists’ role in the national opioid crisis, Rite Aid eventually faced some 1,600 federal, state, and private suits, and had less of a financial cushion than its bigger rivals. Then-CEO Heyward Donigan was trying to bring Rite Aid back to its pharmacist-centric roots—and Bartell’s seemed like a cheap solution. “Who we want to be, more and more, is your local neighborhood pharmacy,” she told the Seattle Times when the deal was announced.
Less than three years later, in January 2023, Donigan stepped down. By October of that year, Rite Aid couldn’t keep up with its losses and filed for Chapter 11 bankruptcy protection to “significantly reduce the company’s debt” while helping to “resolve litigation claims in an equitable manner,” the company said at the time. (Rite Aid, now led by bankruptcy-restructuring specialist Jeffrey Stein, declined to make executives available for an interview.)
While Rite Aid’s bankruptcy is particularly dire among the big chain drugstores, its bigger and more successful rivals are also facing some struggles. (CVS and Walgreens shares are down about 16% and 48%, respectively, over the past year.) “This is not a happy industry in retail,” says Neil Saunders, a retail analyst for GlobalData.
The loss of drugstores means more than just pharmacy deserts. For many low-income and underserved communities, drugstores also serve as groceries and hubs for other necessities. And their closures “can mean that they’re losing what is essentially their access point to a lot of goods and services,” the University of Washington’s Hansen points out.
But wealthier neighborhoods are also seeing some fallout. In Seattle, I met Billy Chow for lunch in the lakeside suburb of Kirkland. He had just been taking calls from some of his former colleagues at Bartell’s who were expecting to lose their jobs: “Rite Aid’s doing another RIF,” Chow told me, using the corporate shorthand for “reduction in force,” or layoffs.
After lunch, Chow walked me past one of the newest and shortest-lived Bartell’s, which he had worked on opening right before the Rite Aid sale. The location seemed ideal, down the street from a large Google campus and all of the high-paid tech employees who would make attractive customers. Yet now the building facade was blank, the windows empty, any evidence of Chow’s work erased. Its closure was a quiet collapse, and a dispiriting end to his 10 years at Bartell’s.
“It was a beautiful fabric,” he says. “And you take one small piece of it and pull—and it all unravels.”
At the end of my week visiting the fresh graves of Seattle’s pharmacies, I finally found a new umbrella. On my way out of town, I stopped at the still-open and well-stocked Bartell’s in Bellevue, the suburb where Jeff Bezos originally founded Amazon. Then I drove five hours southeast to meet another Bartell’s refugee—one who offered a glimmer of hope.
After a gorgeous drive past Washington’s waterfalls and over its snowcapped mountains, through the Yakama Native American Reservation, I wound up on Main Street in the big-sky town of Goldendale, population 3,450. In 2021, Jacqueline Eide, a pharmacist who spent 15 years at Bartell’s (eventually becoming director of retail operations) fled Seattle to buy the town’s 50-year-old corner drugstore, which she renamed Goldendale Pharmacy.
1,500+
CVS, Walgreens, and Rite Aid's announced store closures.
Under its airy brick arches, Eide and her staff sell chocolates and greeting cards along with all the medicines needed by the local extended community of ranchers and farmers.
Since buying Goldendale with two partners, Eide has treated a growing stream of strep throats and animal bites. (“One of the things that you learn in a rural area is that barn cats are not as friendly as you think they are,” she says.)
But while Eide says her business is “stable,” she hasn’t been able to fully escape the industry’s PBM pressures. In January she made a decision that cost her about a third of her business—and forced about 200 of her customers to find another pharmacy: Eide decided not to accept the new insurance those patients had been moved to with the new year, because she would have lost money filling its prescriptions under its PBM’s pricing. “They were reimbursing below my cost, on average,” she says.
Now, Eide says, some of those former patients must fill their prescriptions at the local hospital’s pharmacy, while others have to drive 35 miles to the big chains across the Columbia River and the Oregon state line. And the patients who have tried to fill their prescriptions through their PBM’s preferred mail-order pharmacy have found that it isn’t always a workable solution in remote rural areas. In Goldendale, for example, the mail is routed through Portland, a city 115 miles away. “We had two feet of snow in January, and mail wasn’t getting through,” Eide recalls.
Still, Eide says she’s optimistic about the future of her small pharmacy, and has plans to eventually buy a few more. “I don’t ever want to get too big,” she says. “But I want to see pharmacists be able to do more to ease the burden on the whole health care team.”
It’s a little bit of hope for an industry—and a state, and a nation—that desperately needs some. As Eide says, “Everybody knows we’re broken.”
A version of this article appears in the June/July 2024 issue of Fortune with the headline "The death of the American pharmacy."
This story was originally featured on Fortune.com

 Yahoo Finance
Yahoo Finance 